Ultrasound & Infection Transmission: Is Cleanliness Next to Godliness in our House?
In Dr. Samuel Shem’s House of God, Dr. Samuel Shem paints a satire of mortal physicians given the uncanny ability to change the lives of humans. This caricature of our profession highlights the importance of our day-to-day job on the health of our patients. As providers, we strive to reduce our harm to patients and to treat the diseases that plague them. Ultrasound, too, is a medical technology that comes with adverse effects for patients. Today we will address how various pieces of an ultrasound machine can become contaminated, a categorical approach to cleaning, and special circumstances unique to certain fields of practice.
How clean are probes?
Ultrasound probes have been linked to infectious spread. In May to June 2004, an outbreak of multidrug-resistant Pseudomonas aeruginosa was linked to a defective transesophageal echocardiography probe[1]. A 5mm defect in the surface near the transducer was determined to be the nidus of infection, linked to a common exposure during cardiac surgery. Even outside of the operating room, ultrasound probes still come with inherent risks of bacterial contamination, even after disinfection[2,3]. If probes are known to be this dirty, how often should we be cleaning? What does this involve?
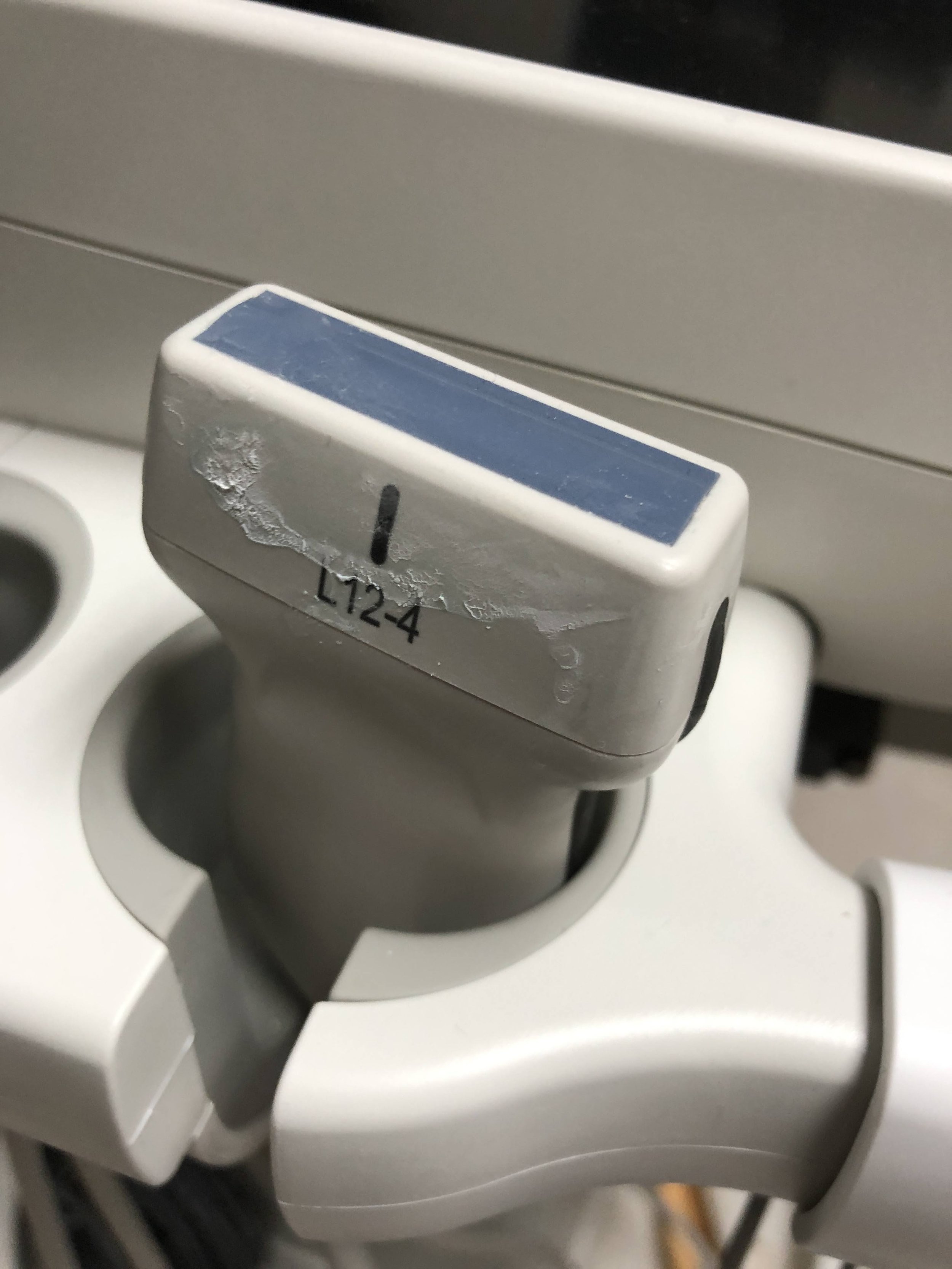
Don’t let your probes get this way! As clinicians, we strive to take the best possible care of our patients and, of course, do no harm.
How can we address the problem?
Designing a maintenance strategy involves multiple facets with many approaches to cleaning. Based on contact with skin or mucous membranes, probes can be categorized into critical, semi-critical, and noncritical based on the Spaulding Classification[4–7] (Table). Furthermore, there are multiple approaches to sterilizing of medical equipment: chemical, thermal, and radiation. Chemical cleaning agents can be low-level disinfectants that will destroy most bacteria. Intermediate disinfectants destroy vegetative bacteria and many viruses. High-level disinfectants are able to remove bacterial spores[4,5]. Chemical selection also depends on cost and availability, based on area of practice and provider resources. Ultraviolet-C (UV-C) radiation has been demonstrated to be both an effective and a time-efficient method of cleaning ultrasound probes[8,9]. Personalizing a hygiene strategy for specific a medical practice requires attention to multiple dimensions beyond the machine itself.
A detailed chart on “Transduce Preparation and Cleaning” is available at this link.
How do I address endocavitary probes?
Today, we will highlight a unique risk factor to pelvic ultrasounds. Endocavitary probes used for transvaginal exams require special viral considerations. Protective barriers with pore sizes less than 30 nanometers should block most viruses, including human papillomavirus (HPV). However studies have shown that probe covers, even with low-level disinfection, may not be sufficient[10].These probes may require UV-C decontamination, which have shown significant efficacy against HPV[11,12]. This is just one example of how a system may augment “low-level disinfection” methods for critical probes.
High-level disinfection varies by practice setting. In a hospital, emergency departments may implement more detailed algorithms, including barrier methods, such as a probe cover or sheath. Additional low-level disinfectant solutions may be implemented for noncritical or semicritical probes. It has also been suggested that alcohol-based wipes may dry out and damage rubber transducers[13]. Cleaning critical probes may require additional resources from central sterile processing. In a smaller clinic or similar low-resource setting, a Trophon may be utilized. This machine utilizes a sonicated disinfectant to clean ultrasound probes, with demonstrated polymicrobial efficacy[14].
How can we keep our house clean?
In every physician’s house, the details of the practice will be unique to location, patient population, equipment, and much more. Implementing an effective strategy requires catering to each practice setting. Resources must be allocated to critical probes, which require high-level disinfection with perhaps additional sterilization techniques. Ultrasound systems have repeatedly demonstrated significant contamination and infection risks to patients. Fortunately, there exists validated methods to address these inherent risks of practicing medicine. Our next topic of discussion will address the risks associated with ultrasound gel use.
Download the Spaulding Classification graphic here.
Authored by Jason Wang DO, MBS
References
1. Seki M, Machida H, Yamagishi Y, Yoshida H, Tomono K. Nosocomial outbreak of multidrug-resistant Pseudomonas aeruginosa caused by damaged transesophageal echocardiogram probe used in cardiovascular surgical operations. J Infect Chemother Off J Jpn Soc Chemother 2013;19(4):677–81.
2. Westerway SC, Basseal JM, Brockway A, Hyett JA, Carter DA. Potential Infection Control Risks Associated with Ultrasound Equipment - A Bacterial Perspective. Ultrasound Med Biol 2017;43(2):421–6.
3. Javaid M, Qasim H, Naseem F, et al. Role of X-ray equipment and ultrasound machines as possible vectors of nosocomial bacteria in the community. J King Saud Univ - Sci 2022;34(6):102154.
4. Guideline for Ultrasound Transducer Cleaning and Disinfection [Internet]. 2021 [cited 2023 Aug 31];Available from: https://www.acep.org/patient-care/policy-statements/guideline-for-ultrasound-transducer-cleaning-and-disinfection
5. Guidelines for Cleaning and Preparing External- and Internal-Use Ultrasound Transducers and Equipment Between Patients as Well as Safe Handling and Use of Ultrasound Coupling Gel [Internet]. Assoc. Med. Ultrasound. 2022 [cited 2023 Aug 31];Available from: https://www.aium.org/resources/official-statements/view/guidelines-for-cleaning-and-preparing-external--and-internal-use-ultrasound-transducers-and-equipment-between-patients-as-well-as-safe-handling-and-use-of-ultrasound-coupling-gel
6. Shokoohi H, Armstrong P, Tansek R. Emergency department ultrasound probe infection control: challenges and solutions. Open Access Emerg Med 2015;7:1–9.
7. Healthcare Equipment | Disinfection & Sterilization Guidelines | Guidelines Library | Infection Control | CDC [Internet]. 2019 [cited 2023 Aug 31];Available from: https://www.cdc.gov/infectioncontrol/guidelines/disinfection/healthcare-equipment.html
8. Bloc S, Mercadal L, Garnier T, et al. Evaluation of a new disinfection method for ultrasound probes used for regional anesthesia: ultraviolet C light. J Ultrasound Med Off J Am Inst Ultrasound Med 2011;30(6):785–8.
9. Kac G, Gueneret M, Rodi A, et al. Evaluation of a new disinfection procedure for ultrasound probes using ultraviolet light. J Hosp Infect 2007;65(2):163–8.
10. Guidelines for Cleaning Transvaginal Ultrasound Transducers Between Patients - PubMed [Internet]. [cited 2023 Aug 31];Available from: https://pubmed.ncbi.nlm.nih.gov/28190623/
11. Pichon M, Lebail-Carval K, Billaud G, Lina B, Gaucherand P, Mekki Y. Decontamination of Intravaginal Probes Infected by Human Papillomavirus (HPV) Using UV-C Decontamination System. J Clin Med [Internet] 2019 [cited 2023 Aug 31];8(11). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6912769/
12. Casalegno J, Le Bail Carval K, Eibach D, et al. High Risk HPV Contamination of Endocavity Vaginal Ultrasound Probes: An Underestimated Route of Nosocomial Infection? PLoS ONE 2012;7(10):e48137.
13. Koibuchi H, Fujii Y, Kotani K, et al. Degradation of ultrasound probes caused by disinfection with alcohol. J Med Ultrason 2001 2011;38(2):97–100.
14. Trophon®2 | Nanosonics [Internet]. [cited 2023 Sep 14];Available from: https://www.nanosonics.us/products/trophon-2/